A workforce under pressure
With increasing pressure on the healthcare workforce, the issue of staff engagement is coming more sharply into focus.
Across all sectors, the physical and mental wellbeing of employees are predictors of desirable organisational outcomes such as effectiveness, productivity and innovation. They can also predict undesirable outcomes such as absenteeism and staff turnover. And in healthcare, employee engagement has further crucial effects on patient safety, quality of patient experience and health outcomes.
Measuring employee wellbeing, attitudes and engagement gives valuable insight into these factors. Cemplicity is known for its deep understanding of the field of Patient-Reported Measures – and increasingly, we are asked about the role of staff in achieving excellent patient experiences and outcomes.
WHO project a shortfall of 18 million healthcare employees by 2030 worldwide. The NHS in England is already short of over 100,000 staff, including 10,000 doctors and 40,000 nurses, official figures show.
The King’s Fund, Nuffield Trust and Health Foundation have said in a joint briefing that “If the emerging trend of staff leaving the workforce early continues and the pipeline of newly trained staff and international recruits does not rise sufficiently, this number could be more than 350,000 by 2030.”
The Quadruple Aim
What strikes us as we expand our work in this field is that while the business case is compelling, it is also simply the right thing to do.
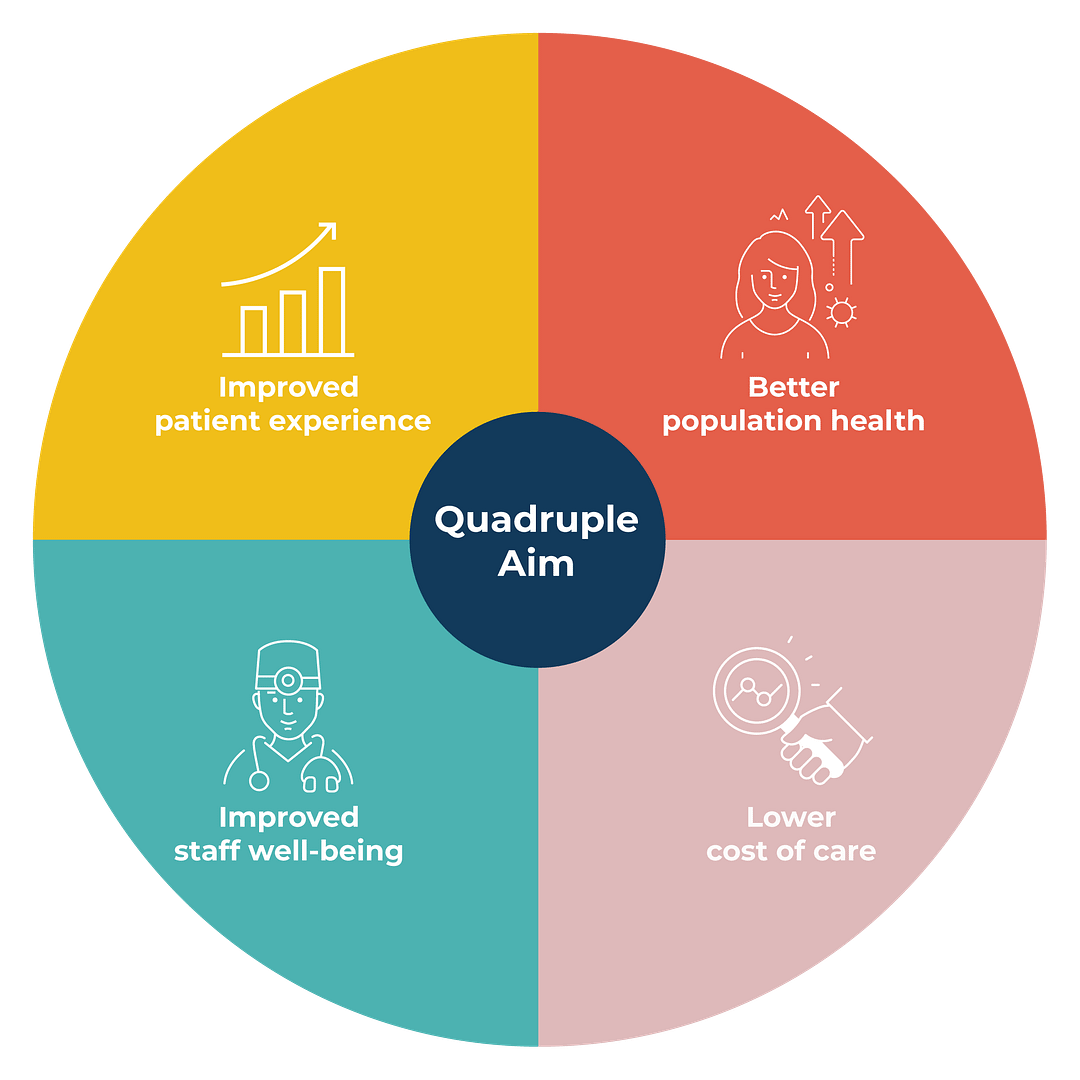
The Quadruple Aim recognises that there can be no health system without dedicated carers. Healthcare workers are reporting unprecedented levels of disengagement, pressure and physical danger yet the Quadruple Aim challenges us to enable our nurses, doctors, and carers to find joy and meaning in their work. We need to care for them, so that ‘they can fulfil their calling of providing outstanding professional care for patients’ (West and Dawson, see below).
In a recent physician survey in the USA, 60% of respondents indicated they were considering leaving practice; 70% of surveyed physicians reported similar findings with approximately 44% of respondents reporting very low or low morale. These findings also extend to the nursing profession. in a 2013 US survey of registered nurses, 51% of nurses worried that their job was affecting their health; 35% felt like resigning from their current job. Similar findings have been reported across Europe, with rates of nursing job dissatisfaction ranging from 11% to 56%. (BMJ Qual Saf 2015;24:608-610)
Employee Engagement and performance
The link between employee wellbeing, engagement and performance is highlighted in a research study by Michael West (Lancaster University) and Jeremy Dawson (University of Sheffield), commissioned by The Kings Fund. It defines engagement, presents evidence linking employee engagement to performance, and touches on some strategies to improve engagement. It also compares the results of the national NHS Staff survey with organisational outcome measures such as staff absenteeism and turnover, patient satisfaction, and mortality and safety measures including infection rates.
Highlights include:
- It is important to ensure a shared understanding of what staff engagement means. A common understanding of engagement includes things like a positive, fulfilling work-related state of mind, proactivity, enthusiasm and initiative, good ‘citizenship’ behaviours and organisation commitment and advocacy. However, when some organisations use the term engagement, they are talking about staff involvement in decision-making and the openness of communication between staff and leadership.
- There is a strong, evidence-based, business case for staff engagement, including:
- Strong links between staff engagement and organisational performance. The analysis shows the impact of a one standard deviation improvement in engagement, which, in 2012, would have led to a £150,000 savings in salary costs for an average acute NHS trust.
- The link between low engagement and burnout (characterised by cynicism, exhaustion and inefficacy). Burnout leads to absenteeism, poor patient experiences and clinical mistakes, so is critical for both organisational outcomes and safety.
- Evidence that in organisations where engagement is higher, mortality is lower.
- In trusts where a large percentage of staff felt they could contribute towards improvements at work, infection rates had decreased.
- Factors that foster good engagement include:
- Well-structured appraisals. A good appraisal sets clear objectives, is helpful in improving how someone does their job and demonstrates that the person is valued.
- Well-structured teams. These have shared objectives, work interdependently and meet regularly to discuss their effectiveness.
- Supportive line management and good job design, with meaningful, clear tasks and the opportunity to be involved in decision-making.
How to measure staff engagement
1. What to ask
The starting point in establishing an effective staff engagement programme is to determine the right questions to ask staff. Here, an organisation’s definition of engagement will be a strong influence on the survey design.
Many organisations ask questions about aspects that are strategically important e.g. leadership, clarity of vision, culture and values. They may also cover staff wellbeing and safety. And they can address factors such as whether staff have effective appraisals and are part of a well-functioning team.
Whatever topics one chooses, there are advantages to using validated questions:
- To have confidence you are measuring factors that, if improved, will impact on staff engagement.
- To avoid the cost of bespoke research services e.g. the need to cognitively test a survey.
- To optimise opportunities to benchmark your results against others.
The NHS staff survey
The NHS staff survey is one of the largest workforce surveys run in the world and has been run every year since 2003. Over 1.1 million people were invited to participate in the most recent survey in 2019, across 300 NHS organisations. The response rate was 48% with 83% of people responding by email.
This survey covers a wide range of staff wellbeing areas. Engagement is measured across three dimensions: psychological engagement (‘I look forward to work’, ‘I am enthusiastic about my job’ and ‘time passes quickly when I am working’); advocacy (‘I would recommend my trust as a place to work’, If a friend or relative needed treatment, I would be happy with the standard of care provided by this trust); and involvement (‘I am able to make suggestions to improve the work of my team/department’, ‘there are frequent opportunities for me to show initiative in my role’ and ‘I am able to make improvements happen in my area of work’.)
The survey also covers other important areas, asking about the safety culture, appraisals, training and development opportunities and bullying.
2. When to ask
Some of our clients prefer to adopt a less frequent surveying cycle, e.g. an annual survey. One benefit of this is that there is plenty of time between survey cycles in which to analyse results, address outlying performance and communicate changes to respondents before asking them to take part again.
However, unless there is a strong reason to do otherwise, Cemplicity encourages clients to consider more continuous surveying approaches. For example, you could survey a sample of staff every month, from across all teams in your organisation, with each staff member only being asked for feedback 1-2 times per year.
The benefit of this approach is that you are aware of issues immediately, rather than up to 12 months after they occur, follow-up actions can be evenly spread across the year and you are able to more quickly see the impact of your improvement initiatives.
3. How to ask
For timeliness, economy and good participation, we recommend starting your survey by email, and only then introducing supporting modes if necessary, e.g. tablets or paper surveys. How a new programme is introduced into the organisation is important and planning the launch and staff communication is a big part of early programme planning.
Improving Staff Engagement
It’s all about improving staff engagement, not just measuring it and a critical success factor is visible leadership.
Company leaders need to be involved in launching the programme to staff, ensuring adequate resources for follow-up and providing active ongoing sponsorship. Helping staff to see what leaders are paying attention to brings a focus to the behaviours that the organisation wishes to promote.
Another critical step is to close the loop. This means allocating enough resource to take action on staff feedback and to communicate changes back to staff. Without this, a programme can lead to greater frustration, lower engagement and an unwillingness to participate in future surveys.
It is valuable to set benchmarks at the start of the programme for factors such as absenteeism, staff turnover, patient mortality and infection rates, and to monitor changes as engagement improves. You may also choose to engage specialist consultants to undertake analysis such as triangulating staff engagement ratings with patient ratings and organisational performance metrics.
Expert advisors can also work with management to address strategic opportunities for improving staff engagement. These can include creating effective appraisal processes, building effective teams, and improving involvement and communication from leadership to staff and vice versa.
In summary, across all industries, substantial evidence links great organisational outcomes to staff wellbeing and engagement. However, nowhere is this more important than in healthcare, where the body of evidence also links workforce wellbeing to patient outcomes and experiences.
Cemplicity’s expertise is in how to optimise participation and deliver insight that is easy to act on. We create timely visibility across organisations and systems, showing you what matters to patients and staff. We can help you to see how you are performing on key measures, and what to focus on to get the greatest improvement. At a time when the healthcare workforce is under growing pressure, our programmes can help organisations get more value from current resources.

